Introduction
- Cholesterol, a type of lipid-a waxy, fat-like substance, is an essential amphipathic sterol, a fundamental component of cellular membranes, serves as a precursor for steroid hormone biosynthesis, and plays a critical role in bile acid metabolism.
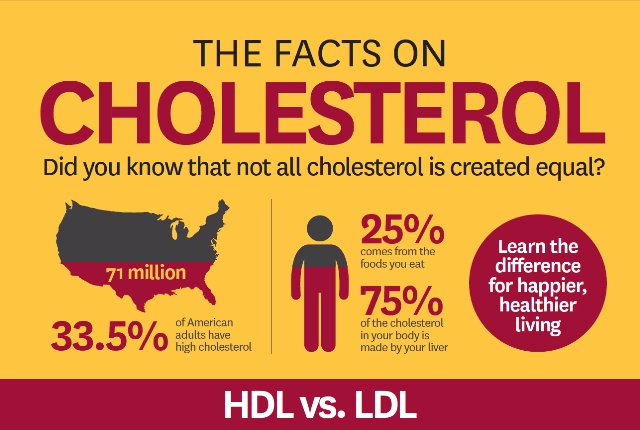
- Cholesterol comes from two sources. Your liver makes all the cholesterol you need. The remainder of the cholesterol in your body comes from foods from animals. For example, meat, poultry and dairy products all contain dietary cholesterol. Those same foods can also be high in saturated and trans fats. These fats can increase the cholesterol in your body. For some people, this added cholesterol means they go from a normal cholesterol level to one that’s unhealthy. Some tropical oils, such as palm oil, palm kernel oil and coconut oil, contain saturated fat that can increase bad cholesterol. These oils are often found in baked goods.
- Despite its indispensable biological functions, dysregulated cholesterol homeostasis, particularly hypercholesterolemia, significantly contributes to atherosclerotic cardiovascular disease (ASCVD), a leading global cause of morbidity and mortality.
- The pathophysiological consequences of elevated low-density lipoprotein (LDL) cholesterol and diminished high-density lipoprotein (HDL) cholesterol extend beyond lipid metabolism, encompassing inflammatory cascades, oxidative stress, endothelial dysfunction, and thrombogenic potential.
-
Cardiovascular disease (CVD) continues to be the leading global cause of morbidity and mortality, with dyslipidemia constituting a primary modifiable determinant of its pathogenesis. The asymptomatic nature of cholesterol perturbations often leads to a delayed diagnosis, necessitating proactive screening, evidence-based therapeutic interventions, and lifestyle modifications to mitigate adverse health outcomes. This discourse elucidates the intricate mechanisms of cholesterol metabolism, delineates the etiological contributors to hypercholesterolemia, examines its systemic ramifications, and evaluates contemporary and emerging management paradigms.
This treatise undertakes an exhaustive analysis of cholesterol’s biochemical roles, its involvement in pathogenic vascular remodeling, and the clinical implications of dyslipidemia.
Furthermore, contemporary pharmacological and non-pharmacological interventions will be examined in light of emerging research in lipidomics, molecular cardiology, and genomics.
The Biochemical and Molecular Roles of Cholesterol
- Cholesterol biosynthesis follows a highly regulated, multi-step enzymatic cascade within the mevalonate pathway, culminating in the endogenous production of cholesterol predominantly in hepatocytes. This tightly controlled process is subject to feedback inhibition via sterol regulatory element-binding proteins (SREBPs), which modulate transcription of the HMG-CoA reductase gene, the rate-limiting enzyme in cholesterol synthesis.
- Beyond its structural function in lipid bilayers, cholesterol participates in lipid raft formation, integral to cell signaling, immune responses, and synaptic transmission.
- Cholesterol also serves as the substrate for cytochrome P450-mediated steroidogenesis, yielding essential hormones such as cortisol, aldosterone, and sex steroids. Additionally, bile acid biosynthesis—mediated by cholesterol 7α-hydroxylase (CYP7A1)—facilitates lipid emulsification and enterohepatic circulation, underscoring cholesterol’s role in digestive physiology.
Lipoprotein Classification and Pathophysiological Implications
Lipoproteins, macromolecular complexes facilitating cholesterol transport, are classified based on their density, apolipoprotein composition, and metabolic fate:
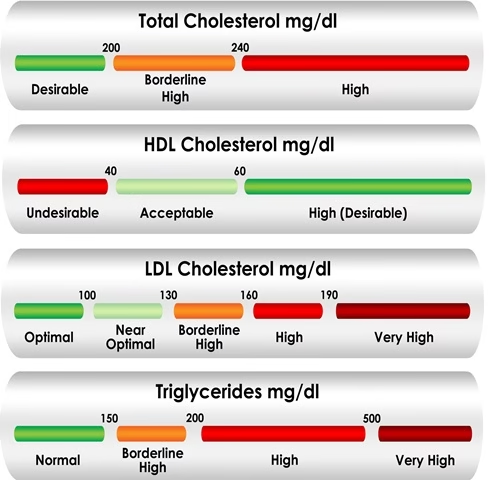
1. Low-Density Lipoprotein Cholesterol (LDL-C): The Atherogenic Cholesterol
LDL particles deliver cholesterol to peripheral tissues via receptor-mediated endocytosis. Excessive circulating LDL, particularly its small dense subclass (sdLDL), undergoes oxidative modification, triggering endothelial dysfunction, foam cell formation, and the initiation of atherosclerotic plaque development. Oxidized LDL (oxLDL) serves as a ligand for scavenger receptors on macrophages, exacerbating pro-inflammatory signaling and lesion instability.
2. High-Density Lipoprotein Cholesterol (HDL-C): The Vasculoprotective Cholesterol
HDL exerts an atheroprotective function primarily through reverse cholesterol transport (RCT), wherein excess cholesterol is effluxed from macrophages and peripheral tissues back to the liver for excretion. HDL-mediated cholesterol efflux, facilitated by ATP-binding cassette transporters ABCA1 and ABCG1, prevents foam cell formation. Moreover, HDL possesses anti-inflammatory, antioxidant, and endothelial-stabilizing properties, further mitigating ASCVD risk.
3.Triglycerides (TGs):
While essential for energy metabolism, excessive TG concentrations, particularly in the context of insulin resistance, exacerbate lipotoxicity, endothelial dysfunction, and pro-inflammatory cascades, intensifying cardiovascular risk.
Maintaining an optimal lipid profile is paramount for sustaining cardiovascular integrity, necessitating timely intervention upon dyslipidemia detection.
Pathophysiology of Dyslipidemia and Atherosclerotic Progression
Hypercholesterolemia initiates a cascade of vascular pathologies, culminating in atherosclerotic plaque formation and cardiovascular sequelae:
- Endothelial Dysfunction: Increased LDL oxidation leads to nitric oxide (NO) depletion, impairing vasodilation and enhancing endothelial permeability to lipoproteins.
- Monocyte Recruitment and Foam Cell Formation: Chemoattractant molecules such as monocyte chemoattractant protein-1 (MCP-1) and adhesion molecules (ICAM-1, VCAM-1) promote monocyte adhesion, infiltration, and differentiation into macrophages, which engulf oxLDL to form foam cells.
- Plaque Progression and Rupture: Continuous lipid accumulation results in fibrous cap formation. However, increased matrix metalloproteinase (MMP) activity destabilizes plaques, predisposing them to rupture and thrombosis.
Etiological Determinants of Hypercholesterolemia
Dyslipidemia manifests from both genetic and environmental influences:
- Monogenic Hyperlipidemia: Familial hypercholesterolemia (FH), an autosomal dominant disorder, arises from mutations in LDLR, APOB, or PCSK9, impairing LDL clearance and precipitating premature ASCVD.
- Polygenic Dyslipidemia: Common lipid disorders stem from multiple genetic variants affecting lipoprotein metabolism, often compounded by lifestyle factors.
- Secondary Dyslipidemia: Insulin resistance, metabolic syndrome, chronic kidney disease, and pharmacologic agents (e.g., glucocorticoids, beta-blockers) exacerbate dyslipidemia through diverse mechanisms.
Hypercholesterolemia arises from a confluence of genetic, lifestyle, and metabolic factors. Identifying and addressing these determinants is central to effective cholesterol management.
1. Dietary Influences
- Excessive intake of saturated and trans fatty acids perturbs hepatic lipid regulatory mechanisms, amplifying endogenous LDL-C synthesis and exacerbating systemic inflammation.
- Diets with a high glycemic load exacerbate hepatic triglyceride production and dyslipidemia via insulin-mediated pathways.
- Inadequate dietary fiber intake impairs enterohepatic cholesterol recirculation, further potentiating hypercholesterolemia.
2. Physical Inactivity and Sedentarism
- Reduced physical activity correlates with diminished lipoprotein lipase activity, impeding HDL-C–mediated cholesterol clearance and exacerbating LDL-C accumulation.
- Sedentarism contributes to adiposity and systemic insulin resistance, compounding dyslipidemic manifestations.
3. Obesity and Metabolic Dysregulation
- Visceral adiposity exacerbates lipotoxicity, insulin resistance, and hepatic VLDL overproduction, propagating atherogenic dyslipidemia.
- Obesity-associated inflammation amplifies systemic oxidative stress and endothelial dysfunction, predisposing individuals to CVD.
- Adipose tissue secretes pro-inflammatory mediators (e.g., TNF-α, IL-6), which perturb hepatic lipid metabolism, exacerbating dyslipidemia.
- Central (visceral) obesity, in particular, is associated with insulin resistance, which perpetuates hypertriglyceridemia and impaired lipid oxidation.
4. Tobacco and Alcohol Consumption
- Cigarette smoke induces oxidative modifications of LDL, exacerbating endothelial dysfunction and accelerating atherogenesis.
- Chronic ethanol intake disrupts hepatic lipid regulation, promoting increased VLDL production and triglyceride accumulation.
5. Genetic and Hereditary Factors
- Monogenic disorders such as familial hypercholesterolemia (FH) result in defective LDL receptor function, necessitating pharmacologic intervention.
- Polygenic influences affect lipid metabolism, modulating individual susceptibility to hypercholesterolemia.
6. Comorbidities and Endocrinopathies
- Endocrine disorders (e.g., hypothyroidism, diabetes mellitus) alter hepatic lipid metabolism, exacerbating dyslipidemia.
- Chronic Renal and hepatic insufficiencies impaired lipid clearance mechanisms further contribute to deranged lipid profiles, necessitating targeted therapeutic strategies.
- CONSEQUENCES OF HIGH CHOLESTEROL
Atherosclerotic Cardiovascular Disease (ASCVD)
High cholesterol is a major risk factor for atherosclerotic cardiovascular disease, which is caused by buildup in the arteries and increases the possibility of heart disease and stroke.
Myocardial Infarction and Cerebrovascular Accidents
High amounts of bad cholesterol in your blood can block a critical path to your brain by clogging up your arteries. Plaque instability and rupture incite thrombogenesis, culminating in acute coronary syndromes and ischemic strokes.
Diabetes
Diabetes can put a dent in your good cholesterol and increase the amount of bad cholesterol in your blood, increasing your risk of heart attack and stroke.
Peripheral Artery Disease
PAD (peripheral artery disease) narrows arteries and reduces blood away from your heart to other parts of your body. High blood cholesterol increases your risk of PAD and can also narrow critical pathways through your arteries. Atherosclerotic obstructions within peripheral vasculature precipitate ischemic manifestations such as intermittent claudication and critical limb ischemia.
Hypertension and Endothelial Dysfunction
High blood pressure can damage your blood vessels, where the bad kind of cholesterol (LDL) can build up and narrow your arteries predisposing individuals to hypertension and increased cardiac afterload. This can impair your circulatory system and put you at a higher risk for life-threatening conditions.
Lower your cholesterol to lower your risks
Lowering LDL cholesterol will lower your risk of health issues like heart attack and stroke. A first step is checking your cholesterol.
Remember lifestyle habits like eating a healthy and balanced diet, moving your body, and eliminating tobacco use can all help you control your cholesterol! Talk to your health care professional about the best treatment plan for you.
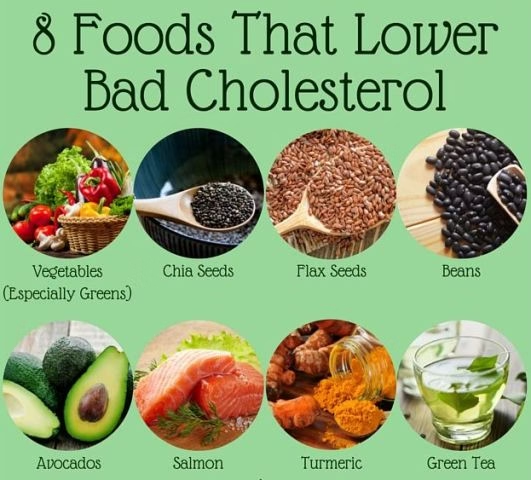
Dietary Recommendations:
| Foods to Eat | Foods to Avoid |
|---|---|
| Fatty fish (salmon, mackerel) | Fried and processed foods |
| Nuts and seeds (walnuts, almonds, flaxseeds) | Full-fat dairy (butter, cream, cheese) |
| Leafy greens (spinach, kale) | Red and processed meats |
| Whole grains (oats, quinoa, brown rice) | Sugary beverages and refined carbohydrates |
| Legumes (lentils, beans, chickpeas) | Hydrogenated oils and trans fats |
| Avocados and olive oil | Fast food and commercially baked goods |
| Berries and citrus fruits | Excessive alcohol consumption |
Strategies for Cholesterol Optimization
A comprehensive lipid-lowering strategy necessitates an integrative approach encompassing dietary interventions, physical activity augmentation, pharmacologic therapies, and innovative lipid-modulating modalities.
Taking proactive steps can help manage cholesterol levels effectively.
1. Adopt a Heart-Healthy Diet
- Increase fiber intake through fruits, vegetables, and whole grains.
- Choose lean proteins like fish and poultry.
- Reduce saturated fats and eliminate trans fats.
2. Regular Exercise
- Engage in at least 30 minutes of moderate exercise daily.
- Activities like brisk walking, cycling, and swimming help boost HDL levels.
3. Maintain a Healthy Weight
- Losing even a small amount of weight can positively impact cholesterol levels.
4. Quit Smoking and Limit Alcohol
- Stopping smoking improves HDL cholesterol within weeks.
- Limit alcohol intake to moderate levels (1 drink/day for women, 2 drinks/day for men).
Treatment for High Cholesterol
If lifestyle changes are insufficient, medications may be required.
1. Statins (HMG-CoA Reductase Inhibitors)
- Commonly prescribed to lower LDL levels.
- Examples: Atorvastatin, Simvastatin.
2. Ezetimibe (Cholesterol Absorption Inhibitors)
- Prevent cholesterol absorption from food reducing circulating LDL-C.
- Example: Ezetimibe.
3. Bile Acid Sequestrants
- Help the body eliminate excess cholesterol.
- Example: Cholestyramine.
4. PCSK9 Inhibitors
- Used for individuals with genetic high cholesterol.
- Example: Alirocumab.
5. Fibrates
- Potentiate peroxisome proliferator-activated receptor (PPAR) activation, reducing triglyceridemia.
- Example: Fenofibrate.
6. Inclisiran (siRNA Therapy)
- Novel RNA-based therapy targeting hepatic PCSK9 expression, significantly lowering LDL-C.
7. Lipoprotein Apheresis
- Extracorporeal LDL removal is employed in severe hypercholesterolemia cases resistant to pharmacotherapy.
8. Lifestyle Adjustments
- Medications work best when combined with a healthy lifestyle.
🌿 Lifestyle Modifications: The Foundation
For most patients, lifestyle changes should be the first-line therapy unless they have very high-risk factors (e.g., familial hypercholesterolemia, secondary prevention after a cardiovascular event).
Key Lifestyle Interventions:
✅ Diet:
- Reduce saturated fats (e.g., red meat, full-fat dairy).
- Increase unsaturated fats (olive oil, nuts, seeds, fatty fish, like salmon).
- Add soluble fiber (oats, legumes, fruits like apples and citrus).
- Consider plant sterols/stanols (from fortified foods).
- Limit refined carbs and added sugars.
✅ Exercise:
- At least 150 minutes of moderate aerobic activity (like brisk walking) or 75 minutes of vigorous activity weekly.
- Include resistance training 2-3 times per week.
✅ Weight Management:
- Achieving a 5-10% weight loss can significantly improve lipid profile.
- Focus on waist circumference reduction as a marker for visceral fat.
✅ Avoid Tobacco & Alcohol Moderation:
- Quit smoking: Major cardiovascular risk factor.
- Limit alcohol: Excessive intake can raise triglycerides.
💊 Pharmacological Interventions: When Lifestyle Isn’t Enough
Despite best efforts, many patients still need medications, especially if they are:
- At high or very high risk (e.g., established ASCVD, diabetes with multiple risk factors, familial hypercholesterolemia).
- Have LDL-C not at target despite lifestyle interventions.
- Have genetic dyslipidemias.
Main Drug Classes:
| Drug Class | Primary Effect | When Used? |
|---|---|---|
| Statins | ↓ LDL (20–60%), ↓ TG (10–20%) | First line for LDL-C lowering. Proven ASCVD risk reduction. |
| Ezetimibe | ↓ LDL (15–20%) | Added if LDL-C remains high on statins. |
| PCSK9 Inhibitors | ↓ LDL (50–60%) | High-risk patients not at target despite statins/ezetimibe. Costly. |
| Fibrates | ↓ TG (30–50%), ↑ HDL (10–20%) | For severe hypertriglyceridemia (>500 mg/dL) to prevent pancreatitis. |
| Omega-3 Fatty Acids | ↓ TG (20–50%) | For severe hypertriglyceridemia. |
| Bempedoic Acid | ↓ LDL (15–20%) | Newer option if statins not tolerated. |
| Niacin | ↓ TG, ↑ HDL, ↓ LDL | Limited use now due to side effects and lack of outcome data. |
🧭 How to Balance the Two Approaches?
| Scenario | Approach |
|---|---|
| Mild dyslipidemia, low ASCVD risk | Start with lifestyle only. Reassess lipids in 3–6 months. |
| Moderate risk, borderline LDL-C elevation | Lifestyle + consider low/moderate-dose statin if target not reached. |
| High risk (e.g., diabetes, multiple risk factors) | Lifestyle + statin upfront. Monitor response and adjust. |
| Very high risk (e.g., prior MI, stroke) | Aggressive pharmacological therapy + lifestyle. May need multiple agents. |
💡 Key Principles to Remember
✅ Lifestyle is always essential — even when medications are started.
✅ Pharmacotherapy should complement, not replace, lifestyle changes.
✅ Regular monitoring of lipid profile, liver function, and muscle symptoms is crucial.
✅ Focus on shared decision-making — empower patients to understand why both strategies matter.
✅ Individualize goals: Think LDL-C targets based on risk but also consider non-HDL cholesterol and ApoB where available.
Prognosis of High Cholesterol
With timely intervention, individuals with high cholesterol can lead healthy lives. However, unmanaged cholesterol increases the risk of life-threatening conditions. Regular screenings, lifestyle changes, and adherence to treatment plans significantly improve prognosis.
Comparison of Cholesterol Medications
| Medication Type | Function | Common Examples |
|---|---|---|
| Statins | Lower LDL | Atorvastatin, Simvastatin |
| Absorption Inhibitors | Reduce cholesterol absorption | Ezetimibe |
| Bile Acid Sequestrants | Help body eliminate cholesterol | Cholestyramine |
| PCSK9 Inhibitors | Lower genetic high cholesterol | Alirocumab |
Takeaways
- High cholesterol is a silent threat that can lead to severe health issues.
- Lifestyle modifications significantly impact cholesterol levels.
- Regular screening is essential for early detection.
- Medications may be necessary for those at high risk.
Conclusion
Lipid regulation constitutes a cornerstone of CVD prevention, necessitating a proactive, multidisciplinary approach encompassing dietary refinement, structured physical activity, and pharmacologic intervention. As molecular therapies and precision medicine continue to evolve, future cholesterol management strategies are poised to undergo transformative innovations, potentially revolutionizing the trajectory of ASCVD prevention and treatment. Vigilant screening, early therapeutic initiation, and sustained adherence to lipid-lowering interventions remain imperative in mitigating the global burden of dyslipidemia-related morbidity and mortality.
Cholesterol management is crucial for overall health and longevity. By adopting a heart-healthy lifestyle, undergoing regular check-ups, and considering medical interventions, when necessary, individuals can prevent complications associated with high cholesterol. Prioritizing cholesterol control today ensures a healthier tomorrow.
FAQs
1. Can young people have high cholesterol?
Yes, lifestyle and genetics can cause high cholesterol in young individuals.
2. How often should I check my cholesterol levels?
Adults should have a lipid profile test every 4-6 years or more frequently if at risk.
3. Can diet alone lower cholesterol?
Diet plays a significant role, but some may need medications for effective control.
4. Does exercise help in lowering cholesterol?
Yes, regular physical activity increases HDL (good cholesterol) and reduces LDL.
5. Are cholesterol medications safe for long-term use?
Most cholesterol-lowering medications are safe when taken as prescribed by a doctor.
6. Can high cholesterol be reversed?
Yes, through lifestyle changes and medical interventions, cholesterol levels can improve.
7. How often should I get a cholesterol test?
When and how often you should get a cholesterol test depends on your age, risk factors, and family history. The general recommendations are:
For people who are age 19 or younger:
- The first test should be between ages 9 to 11
- Children should have the test again every 5 years
- Some children may have this test starting at age 2 if there is a family history of high cholesterol, heart attack, or stroke
For people who are ages 20 to 65:
- Younger adults should have the test every 5 years
- Men ages 45 to 65 and women ages 55 to 65 should have it every 1 to 2 years
For people older than 65:
- They should be tested every year
References
- American Heart Association. (2023). Understanding Cholesterol.
- National Institutes of Health. (2022). Managing High Cholesterol.
- Mayo Clinic. (2023). High Cholesterol: Symptoms and Causes.
- Centers for Disease Control and Prevention. (2023). Cholesterol Facts.
- Harvard Health Publishing. (2023). The Truth About Fats.
- World Health Organization. (2022). Cardiovascular Diseases Prevention.
- Journal of Lipid Research. (2023). Advances in Cholesterol Treatment.
Further Reading
For an advanced exploration of lipid metabolism and contemporary therapeutic innovations:
- Ference BA, et al. (2017). The Lancet 390(10106): 2510-2520.
- Ridker PM, et al. (2018). New England Journal of Medicine 379(14): 1317-1328.
- Grundy SM, et al. (2019). Circulation 139(25): e1082-e1143.
- Reiner Ž. (2017). European Journal of Preventive Cardiology 24(3_suppl): 6-15.
- Ray KK, et al. (2019). Journal of the American College of Cardiology 74(12): 1572-1585.
- Pencina MJ, et al. (2014). JAMA 311(21): 2203-2214.
- Mach F, et al. (2020). European Heart Journal 41(1): 111-188.
- American Heart Association Guidelines (www.heart.org)

Can you be more specific about the content of your enticle? After reading it, I still have some doubts. Hope you can help me.
Your article helped me a lot, is there any more related content? Thanks!
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article.
Thanks for sharing. I read many of your blog posts, cool, your blog is very good.
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
Thanks for sharing. I read many of your blog posts, cool, your blog is very good.
Your article helped me a lot, is there any more related content? Thanks!
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
Very insightful analysis on cholesterol and its impact on cardiovascular health. The detailed breakdown of LDL, HDL, and their roles in atherosclerosis is particularly enlightening. It’s fascinating how HDL’s atheroprotective functions go beyond just cholesterol transport, offering anti-inflammatory and antioxidant benefits. The discussion on oxidized LDL and its role in endothelial dysfunction raises important questions about early intervention strategies. I wonder if there are emerging therapies targeting sdLDL specifically to prevent its oxidative modification? Also, how do lifestyle factors like diet and exercise influence the balance between LDL and HDL in a clinically significant way? The emphasis on maintaining an optimal lipid profile is crucial, but I’m curious about the challenges in implementing these strategies in diverse populations with varying access to healthcare. What are your thoughts on the role of personalized medicine in managing dyslipidemia? Would love to hear more about how genomics and lipidomics are shaping future treatments.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.
Interesting read! The detailed analysis of cholesterol’s role in vascular health is quite enlightening. I found the part about LDL oxidation and its impact on atherosclerosis particularly compelling. The emphasis on HDL’s protective functions through reverse cholesterol transport is also noteworthy. However, I wonder if the current pharmacological interventions are sufficient to address the complexities of dyslipidemia, especially with the rise of personalized medicine. Could advancements in lipidomics and genomics lead to more targeted therapies in the near future? Also, how effective are non-pharmacological interventions compared to drugs in managing lipid profiles? Would love to hear your thoughts on this!
Thanks for sharing. I read many of your blog posts, cool, your blog is very good.
This is a highly informative and detailed analysis of cholesterol’s role in health and disease. The focus on LDL, HDL, and triglycerides provides a comprehensive understanding of their impact on cardiovascular health. The discussion on oxidative modification of LDL and its role in atherosclerosis is particularly compelling. It’s interesting how HDL’s atheroprotective functions are highlighted, especially its role in reverse cholesterol transport. The emphasis on timely intervention for dyslipidemia is crucial, as it underscores the importance of early detection and management. However, I wonder if the text could delve deeper into the practical applications of these findings in everyday clinical practice. How can healthcare providers better integrate lipidomics and genomics into routine patient care? What are the most effective strategies for patients to maintain an optimal lipid profile? This seems like a critical area for further exploration.
This is a highly detailed and informative analysis of cholesterol’s role in cardiovascular health. The focus on LDL, HDL, and their biochemical pathways provides a clear understanding of their impact on atherosclerosis. The mention of pharmacological and non-pharmacological interventions is particularly relevant, given the growing emphasis on personalized medicine. However, I wonder if the text could delve deeper into the practical applications of lipidomics and genomics in everyday clinical practice. How do these emerging fields translate into actionable strategies for patients? The emphasis on HDL’s atheroprotective function is compelling, but are there any recent studies challenging or expanding this view? Overall, this is a solid foundation, but I’d love to see more discussion on how these insights can be integrated into preventive care. What are your thoughts on the balance between pharmacological and lifestyle interventions in managing dyslipidemia?
Please have a look at the article again. I have added a paragraph regarding balance between lifestyle changes and pharmacological interventions in managing dyslipidemia. Thanks for your concerns.
Please feel free to have any question in your mind.
This is a highly detailed and scientific analysis of cholesterol and its impact on cardiovascular health. The text delves into the biochemical mechanisms, the role of lipoproteins, and the clinical implications of dyslipidemia. It’s fascinating how LDL and HDL play such contrasting roles in vascular health, with LDL contributing to plaque formation and HDL offering protection through reverse cholesterol transport. The mention of oxidative modification of LDL and its role in endothelial dysfunction is particularly intriguing. I wonder, though, how practical it is to monitor and manage these specific lipoprotein subclasses in a clinical setting? The emphasis on maintaining an optimal lipid profile is clear, but what are the most effective non-pharmacological interventions for achieving this? Also, how does emerging research in lipidomics and genomics influence current treatment protocols? This text really highlights the complexity of cardiovascular health, but it also leaves me curious about the real-world application of these findings. What are your thoughts on balancing pharmacological and lifestyle interventions in managing dyslipidemia?
This is a highly informative and detailed analysis of cholesterol’s role in cardiovascular health. The focus on LDL, HDL, and their impact on atherosclerosis is particularly compelling. I appreciate the emphasis on both pharmacological and non-pharmacological interventions, as it highlights the importance of a holistic approach to managing dyslipidemia. The discussion on HDL’s atheroprotective functions and its role in reverse cholesterol transport is fascinating and underscores the complexity of lipid metabolism. However, I wonder if the text could delve deeper into the practical implications of these findings for everyday health management. For instance, how can individuals effectively monitor and optimize their lipid profiles in real-world settings? What are the most accessible and impactful lifestyle changes to reduce cardiovascular risk? This is a great read, but I’d love to hear more actionable insights! What’s your take on integrating these findings into public health strategies?
This treatise provides a comprehensive overview of cholesterol’s role in cardiovascular health, emphasizing both its biochemical functions and pathological implications. The detailed exploration of LDL and HDL dynamics, along with their impact on atherosclerosis, is particularly insightful. The discussion on pharmacological and non-pharmacological interventions highlights the importance of personalized approaches in managing dyslipidemia. However, I wonder if more attention could be given to the role of lifestyle factors, such as diet and exercise, in modulating these processes. The relevance of emerging research fields like lipidomics and genomics in shaping future therapies is intriguing. How might advancements in these areas translate into more effective clinical practices? Overall, this analysis underscores the critical need for early detection and intervention in maintaining cardiovascular health. Do you think current screening methods and public awareness are sufficient to address the global burden of dyslipidemia?
This is a highly detailed and technical analysis of cholesterol and its impact on cardiovascular health. The focus on LDL, HDL, and triglycerides provides a comprehensive understanding of their roles in vascular health. The mention of oxidative modification of LDL and its contribution to atherosclerosis is particularly intriguing. The discussion on HDL’s atheroprotective functions, including reverse cholesterol transport, highlights its importance in mitigating cardiovascular risks. The emphasis on maintaining an optimal lipid profile underscores the need for early intervention in dyslipidemia. However, I wonder how practical it is to implement these findings in everyday clinical practice, especially with the complexity of lipidomics and genomics. Do you think current pharmacological interventions are sufficient to address the multifaceted nature of dyslipidemia, or is there a need for more personalized approaches?
This is a highly detailed and informative piece on the role of cholesterol and lipids in cardiovascular health. The discussion on LDL, HDL, and TG is thorough, but it leaves me wondering—how accessible are these pharmacological and non-pharmacological interventions for the average person?
The focus on HDL’s atheroprotective function is intriguing, especially its anti-inflammatory and antioxidant properties. However, I’m curious—does the average diet or lifestyle support HDL’s beneficial effects, or is it predominantly reliant on medical interventions?
The explanation of oxLDL’s role in atherosclerosis is compelling, yet it raises the question—how effectively can we currently reverse or halt this oxidative process in clinical practice?
The emphasis on maintaining an optimal lipid profile is crucial, but I wonder—what specific lifestyle changes or biomarkers should individuals prioritize for prevention?
Overall, this text underscores the complexity of lipid metabolism and its cardiovascular implications. Do you think current public health messaging is clear enough to help people understand and act on these risks?
This treatise provides a comprehensive exploration of cholesterol’s biochemical roles and its impact on vascular health. The detailed examination of LDL and HDL functionalities offers valuable insights into their contributions to cardiovascular diseases. The discussion on oxidized LDL and its role in atherosclerotic plaque development is particularly enlightening. I appreciate the focus on both pharmacological and non-pharmacological interventions, which underscores the importance of a holistic approach to managing dyslipidemia. However, could you elaborate on how emerging research in lipidomics and genomics might shape future treatments? The emphasis on maintaining an optimal lipid profile is crucial, but how do you suggest we improve public awareness and early detection of dyslipidemia? This analysis is a vital resource for understanding cardiovascular health, but do you think lifestyle changes alone can suffice in managing hypercholesterolemia, or is medical intervention always necessary?
This text provides a comprehensive and detailed overview of cholesterol’s biochemical roles and its impact on cardiovascular health. The emphasis on LDL, HDL, and triglycerides clearly highlights the complexity of lipid metabolism and its clinical implications. The discussion on oxidized LDL and its role in atherosclerosis is particularly intriguing, as it underscores the importance of addressing oxidative stress in cardiovascular disease prevention. I wonder, though, how feasible it is to implement these interventions in routine clinical practice, especially in resource-limited settings. The mention of HDL’s anti-inflammatory and antioxidant properties is reassuring, but how effective are current therapies in enhancing HDL functionality? Also, could emerging research in lipidomics and genomics lead to more personalized treatment approaches for dyslipidemia? Overall, this is an insightful read, but it raises the question of how to bridge the gap between advanced scientific understanding and practical healthcare delivery.
We have integrated libersave into our regional voucher system. It’s fantastic how easily it allows us to consolidate various providers on a single platform.
This treatise provides a thorough and detailed exploration of cholesterol’s role in cardiovascular health. It’s fascinating how it delves into both the biochemical mechanisms and the clinical implications of dyslipidemia. The focus on LDL and HDL, particularly their metabolic pathways and impact on atherosclerosis, is incredibly insightful. However, I wonder if the discussion could expand on the practical application of these findings in everyday clinical practice. Additionally, how do you see the role of emerging research in genomics and lipidomics shaping future interventions? The mention of pharmacological and non-pharmacological interventions leaves me curious about specific examples or case studies that highlight their effectiveness. Overall, this is a compelling read that underscores the importance of lipid management in preventing cardiovascular diseases.
We have integrated libersave into our regional voucher system. It’s amazing how easily it brings together different providers on a single platform.
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
Your article helped me a lot, is there any more related content? Thanks!
Your article helped me a lot, is there any more related content? Thanks!
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article.
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
Your article helped me a lot, is there any more related content? Thanks!
Thanks for sharing. I read many of your blog posts, cool, your blog is very good.
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article.
Your article helped me a lot, is there any more related content? Thanks!
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?